Fantastic Tips About How To Treat A Fib
 Treating Atrial Fibrillation (A Fib) involves a multifaceted approach, combining both theoretical knowledge and practical steps for managing the condition. A Fib is a heart rhythm disorder where the upper chambers of the heart (atria) beat irregularly, leading to a rapid and erratic heartbeat. This increases the risk of stroke, heart failure, and other complications. Treating A Fib requires understanding the underlying causes, symptoms, and the tools available for management. Let's break this down step-by-step and apply theory to practice in a mindblowing way!
Treating Atrial Fibrillation (A Fib) involves a multifaceted approach, combining both theoretical knowledge and practical steps for managing the condition. A Fib is a heart rhythm disorder where the upper chambers of the heart (atria) beat irregularly, leading to a rapid and erratic heartbeat. This increases the risk of stroke, heart failure, and other complications. Treating A Fib requires understanding the underlying causes, symptoms, and the tools available for management. Let's break this down step-by-step and apply theory to practice in a mindblowing way!
Step 1: Assess the Situation (Diagnosis)
- Theory: A thorough understanding of the patient's symptoms, medical history, and risk factors (like high blood pressure, heart disease, diabetes) helps in identifying A Fib early. Diagnosing involves recognizing the irregular heart rhythm and assessing the underlying cause.
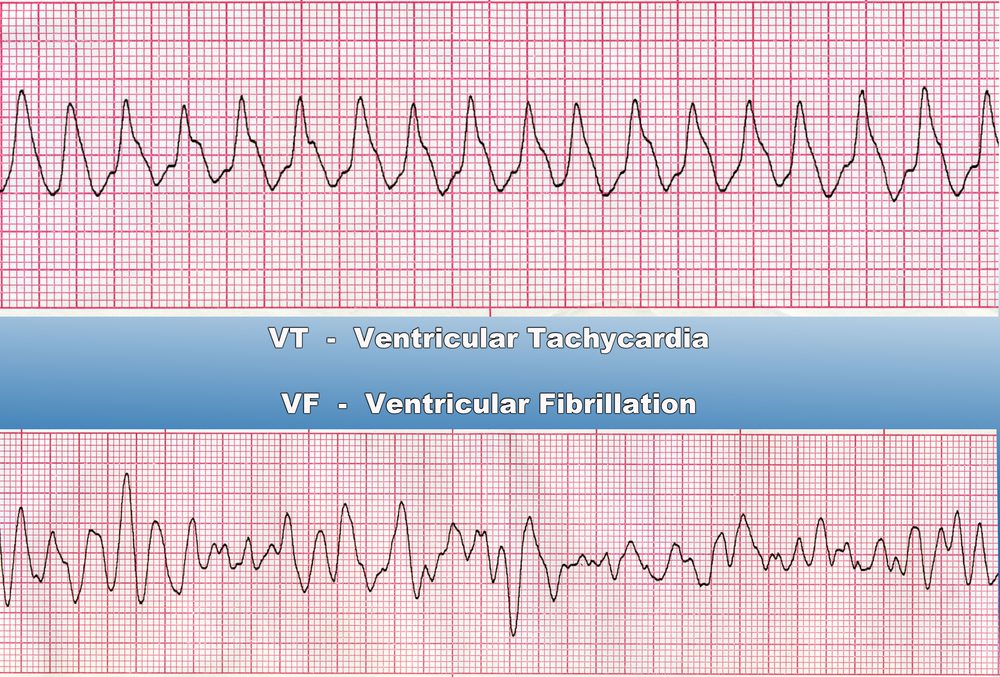
- Application: In practice, this begins with an electrocardiogram (ECG) or Holter monitor to confirm the presence of A Fib. Clinicians also evaluate blood tests and echocardiograms to understand heart function. The more precise the diagnosis, the better the treatment decisions will be. If the cause is reversible (e.g., hyperthyroidism or sleep apnea), addressing that condition could reverse A Fib.
Step 2: Control the Heart Rate (Rate Control)
- Theory: One of the first lines of treatment is to control the heart rate to prevent complications like heart failure. Medications can be used to slow the heart rate without affecting the rhythm.
- Application: In practice, this is done with drugs such as:
- Beta-blockers (e.g., metoprolol) or calcium channel blockers (e.g., diltiazem) to control the heart rate by slowing down the electrical impulses.
- Digoxin can be used in certain cases, especially if the patient has heart failure.
- The goal is to achieve a resting heart rate of 60-100 beats per minute while preventing symptoms like fatigue, shortness of breath, or dizziness. This helps improve the patient's quality of life.
Step 3: Rhythm Control (Restoring Normal Rhythm)
- Theory: The idea here is to convert the irregular heart rhythm back to normal, called sinus rhythm, which is the ideal condition for the heart. This can be achieved through pharmacological or electrical methods.
- Application: In practice, this is approached in two ways:
- Antiarrhythmic medications like amiodarone, flecainide, or sotalol are used to restore and maintain sinus rhythm. They target the electrical pathways in the heart to stabilize the rhythm.
- Electrical cardioversion is a procedure where a controlled electric shock is applied to the heart to reset its rhythm. This is particularly useful when medications are ineffective.
- The effectiveness of this step depends on the duration and severity of the A Fib and whether structural damage to the heart has occurred.
Step 4: Prevent Stroke (Anticoagulation Therapy)
- Theory: Atrial fibrillation significantly increases the risk of blood clots forming in the atria, which can then travel to the brain, causing a stroke. Therefore, blood thinners are essential in reducing this risk.
- Application: In practice, anticoagulants like warfarin or newer direct oral anticoagulants (DOACs) like dabigatran, rivaroxaban, or apixaban are prescribed. The decision is based on a risk scoring system called the CHA2DS2-VASc score:
- C: Congestive heart failure
- H: Hypertension
- A: Age > 75 years
- D: Diabetes
- S2: Stroke history
- V: Vascular disease
- A: Age 65-74 years
- Sc: Sex category (female)
Step 5: Address Underlying Conditions
- Theory: Treating underlying or contributing factors like hypertension, obesity, or sleep apnea can prevent A Fib from recurring and improve long-term outcomes.
- Application: In practice, this involves:
- Lifestyle changes such as weight loss, reducing alcohol intake, and managing stress.
- Controlling hypertension with medications like ACE inhibitors, ARBs, or diuretics.
- Managing sleep apnea with CPAP machines.
- Treating other structural heart issues like valvular heart disease or coronary artery disease. For example, a patient with A Fib due to mitral valve disease might need valve repair or replacement.
Step 6: Long-Term Management (Surveillance and Follow-up)
- Theory: Long-term management focuses on monitoring for recurrence, adjusting medications, and ensuring the patient is not at risk for complications like stroke or heart failure.
- Application: In practice, regular follow-ups are necessary to:
- Monitor blood pressure, heart rate, and anticoagulant therapy.
- Perform periodic ECGs or Holter monitoring to detect recurrences.
- Adjust medications based on efficacy, side effects, or interactions.
- Ensure the patient understands lifestyle changes and the importance of adherence to treatment.
Step 7: Advanced Interventions (If Necessary)
- Theory: When other treatments fail, more invasive options like catheter ablation can be considered. This procedure destroys the heart tissue responsible for the abnormal electrical impulses, offering a potential long-term solution.
- Application: In practice:
- Catheter ablation involves threading a catheter through the veins to the heart, where radiofrequency energy is used to destroy the tissue causing A Fib.
- This is a more permanent solution for patients with persistent or symptomatic A Fib who don’t respond to medications.
Step 8: Empower the Patient
- Theory: Education and shared decision-making are crucial for ensuring patients follow through with their treatment plans and lifestyle changes. Knowledge empowers them to manage their condition and reduce the risk of complications.
- Application: In practice, this involves:
- Educating the patient on symptom monitoring, medication adherence, and recognizing early signs of complications (e.g., stroke).
- Encouraging regular exercise, a heart-healthy diet, and stress management techniques.
Conclusion: Integration of Knowledge into Action
This process requires the combination of scientific understanding, clinical expertise, and patient engagement. By focusing on personalized treatment—balancing heart rate, rhythm control, anticoagulation therapy, and addressing underlying conditions—the theory of A Fib treatment translates into real-world success. Each step builds on the other, showing how multiple strategies converge to offer optimal care and minimize risks. By continuously evolving the approach based on patient response, we enter a cycle of continuous improvement, much like Kaizen (constant small improvements) applied in healthcare!
Pin On Low Sodium And Afib
Do You Know The Warning Signs Of Afib? Trendradars
Ventriculaire Tachycardie Symptomen Oorzaken Diagnose Behandeling

About T. Treat Ltd


Comments
Post a Comment